In this article
- What’s the Link Between Thyroid Conditions and Depression?
- What the Research Says
- Hyperthyroidism and Mental Health: When Overactivity Overwhelms
- Hypothyroidism and Depression: When Sluggishness Shadows Mood
- Why This Matters
- The Takeaway
- Common Symptoms
- The Problem with Misdiagnosis
- Thyroid Medication and Depression
- The Final Word
Did you know that thyroid disorders affect millions of lives worldwide, yet over 60% of cases go undiagnosed? This small, butterfly-shaped gland at the front of your throat is much more than a regulator of metabolism—it’s intricately tied to your mental health, influencing mood, energy levels, and even cognitive function.
In India, where unipolar depression (UD) impacts 3% to 16.9% of the population, research has uncovered a striking connection between thyroid dysfunction and depression. For instance, a landmark study from Kanpur revealed that individuals with UD had significantly higher thyroid-stimulating hormone (TSH) levels compared to healthy individuals. This underscores the critical role of thyroid screening in managing mental health conditions.
Interestingly, the overlap of symptoms like fatigue, low energy, and mood swings often leads to misdiagnosis. While hypothyroidism is commonly linked to symptoms of lethargy and depression, hyperthyroidism is associated with anxiety and irritability. This complex interplay between thyroid hormones and mental health highlights the need for an integrated approach to diagnosis and treatment (source).
In this blog, we’ll uncover the fascinating connection between thyroid disorders and mental well-being, explore how thyroid health impacts mood and cognitive function, and emphasize the importance of timely and accurate diagnosis for better patient outcomes.
What the Research Says

The link between thyroid conditions and mental health is as fascinating as it is complex. For decades, researchers have observed how thyroid imbalances—whether overactive or underactive—can significantly impact emotional and cognitive well-being. In today’s world, where rates of anxiety and depression are soaring, understanding this connection has never been more critical.
Hyperthyroidism and Mental Health: When Overactivity Overwhelms

Did you know that up to 60% of people with hyperthyroidism struggle with clinical anxiety, and an even greater 69% experience symptoms of depression (source)? Hyperthyroidism, caused by an overactive thyroid, doesn’t just rev up your metabolism—it can wreak havoc on your emotional balance, contributing to mood swings, irritability, and even bipolar depression.
A study in the Biological Psychiatry Journal uncovered a possible connection between thyroiditis and a genetic predisposition to bipolar disorder (source). However, this link remains inconsistent, calling for further research to unravel the exact relationship.
To complicate matters, lithium, a common treatment for bipolar disorder, can trigger or worsen hyperthyroidism (source). This dual effect highlights the importance of monitoring thyroid function in patients receiving mood disorder treatments, ensuring that the cure doesn’t aggravate the condition.
Hypothyroidism and Depression: When Sluggishness Shadows Mood

On the flip side, hypothyroidism, an underactive thyroid, has been consistently associated with clinical depression. When the thyroid fails to produce enough hormones, the central nervous system suffers, resulting in symptoms like fatigue, weight gain, and low energy levels (source). These symptoms can mimic or amplify the effects of depression, making it challenging to distinguish between the two conditions.
According to a study in The Biological Psychiatry Journal, individuals with untreated hypothyroidism face a significantly higher risk of developing depressive symptoms (source). This underscores the need for early diagnosis and intervention to address both the physical and emotional impacts of thyroid dysfunction.
Why This Matters
Thyroid disorders are more than just physical health concerns—they can profoundly affect your mental health as well. If you or someone you know is struggling with unexplained mood swings, persistent anxiety, or depression, it may be time to look deeper. Thyroid function testing could reveal an underlying cause, unlocking the potential for more targeted and effective treatment.
The Takeaway
Whether it’s the overactivity of hyperthyroidism fueling anxiety or the sluggishness of hypothyroidism intensifying depression, thyroid imbalances play a critical role in mental health. By prioritizing comprehensive screenings and tailored treatments, individuals can regain control of both their physical and emotional well-being, paving the way for a healthier, more balanced life.
Common Symptoms

Thyroid disorders often mimic the symptoms of mental health conditions, making diagnosis a challenge. Let’s break down the symptoms associated with hyperthyroidism and hypothyroidism and how they overlap with conditions like anxiety, bipolar depression, and cognitive dysfunction.
Hyperthyroidism Symptoms: When Overactivity Mirrors Anxiety
If you have hyperthyroidism, your symptoms may feel eerily similar to those of clinical anxiety or bipolar depression. These include:
- Insomnia
- Anxiety
- Elevated heart rate
- High blood pressure
- Mood swings
- Irritability
Hyperthyroidism revs up your body’s processes, often leaving you feeling emotionally and physically out of control.
Hypothyroidism Symptoms: When Sluggishness Mimics Depression
On the other hand, hypothyroidism shares symptoms with clinical depression and cognitive dysfunction—a condition involving memory loss and difficulty processing thoughts. Common symptoms include:
- Bloating
- Weight gain
- Memory loss
- Difficulty processing information
- Fatigue
Hypothyroidism slows down your body’s functions, leading to feelings of lethargy and mental fog.
The Problem with Misdiagnosis

The significant overlap between thyroid conditions and mood disorders can result in misdiagnosis. If you’ve been diagnosed with a mental health condition but have an undiagnosed thyroid disorder, doctors might overlook the root cause.
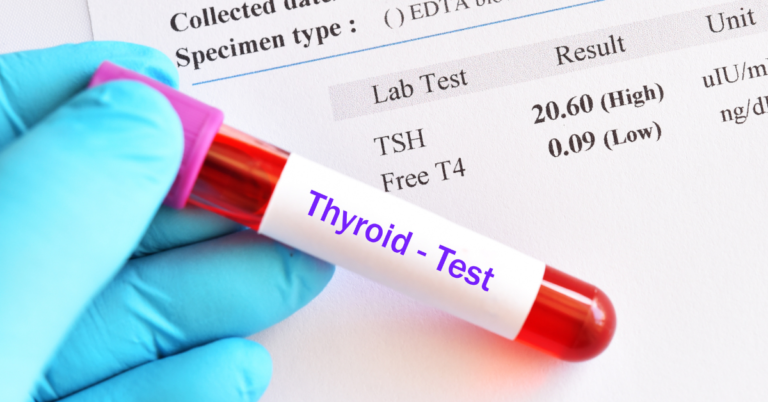
What’s more, even if you undergo a thyroid-stimulating hormone (TSH) test, it may not reveal the full picture. While TSH levels are often used to assess thyroid health, testing T3 and T4 hormone levels can provide a more comprehensive understanding. These hormones are specific indicators of thyroid function that other blood tests might miss.
Why This Matters
Understanding the subtle yet significant connection between thyroid disorders and their overlapping symptoms is crucial for accurate diagnosis and effective treatment. If you’re experiencing unexplained mood swings, memory issues, or persistent fatigue, consider asking your doctor for a complete thyroid panel, including TSH, T3, and T4 levels.
Thyroid Medication and Depression: Navigating the Complex Interplay

The connection between thyroid medication and depression is both intricate and often misunderstood. While thyroid hormone replacement therapy is essential for managing hypothyroidism, it can interact with psychiatric medications, creating unique challenges for those dealing with both conditions. Understanding this interplay is key to ensuring effective treatment for both thyroid dysfunction and mental health.
Thyroid Hormone Replacement: A Vital Yet Intricate Solution
Thyroid hormone replacement therapy, such as levothyroxine, is the gold standard for treating hypothyroidism. By restoring thyroid hormone levels, it alleviates symptoms like fatigue, cognitive difficulties, and depression. However, when combined with antidepressants, it can lead to unique challenges that require careful management.
Research indicates that some antidepressants, including SSRIs and tricyclic antidepressants, can influence thyroid hormone levels by altering their metabolism or uptake (source). This interaction often necessitates adjustments in thyroid medication dosages to maintain therapeutic efficacy.
How Depression Medications Affect Thyroid Function
The interplay between psychiatric medications and thyroid function is a two-way street. While thyroid treatments can impact mental health, medications for depression and mood disorders can also disrupt thyroid activity.
Lithium:
- Commonly prescribed for bipolar depression, lithium is well-known for its effects on thyroid health.
- It inhibits thyroid hormone synthesis and release, potentially causing conditions like hypothyroidism, hyperthyroidism, or even goiter (source).
Antidepressants:
- Medications such as tricyclic antidepressants and SSRIs may interfere with thyroid hormone absorption or metabolism, reducing the effectiveness of thyroid replacement therapy.
These interactions highlight the importance of routine thyroid testing and medication adjustments to address potential imbalances effectively.
Striking the Right Balance: Personalized Treatment Plans
For those navigating the dual challenge of thyroid dysfunction and depression, a personalized treatment approach is essential:
- Regular Thyroid Function Testing: Routine checks of TSH, T3, and T4 levels help identify interactions early.
- Medication Adjustments: If mood stabilizers or antidepressants impact thyroid function, providers may adjust dosages or explore alternatives.
- Close Lithium Monitoring: Frequent thyroid assessments are critical for patients on lithium to detect and manage side effects like hypothyroidism or goiter.
A Word of Caution: Misdiagnosis Risks
The overlapping symptoms of thyroid dysfunction and depression can lead to misdiagnosis. Comprehensive evaluations—combining thyroid function tests with mental health assessments—are crucial for accurate diagnoses and effective care.
The Takeaway
Thyroid hormone replacement therapy can dramatically improve quality of life for individuals with hypothyroidism. However, its interaction with psychiatric medications adds a layer of complexity that requires careful attention. Whether it’s lithium affecting thyroid function or antidepressants altering hormone absorption, a holistic approach—informed by regular testing and collaborative care—ensures the best outcomes for your mental and physical health.
The Final Word: Is Your Thyroid the Missing Piece in Your Mental Health Puzzle?
If you’ve been battling depression, anxiety, or persistent mood swings, it might be time to consider your thyroid health as part of the bigger picture. Even if your TSH levels seem normal, they don’t always tell the whole story. Comprehensive testing of your T3 and T4 hormone levels could uncover hidden thyroid issues affecting your mental well-being.
Take charge of your health by having a candid conversation with your general practitioner, family doctor, or even a mental health professional. Advocate for a full thyroid panel that includes T3 and T4 tests—it’s a small step that could make a big difference in getting the right diagnosis and treatment.
A word of caution: never stop or adjust your mental health medications without consulting your doctor. If you’re curious about alternative treatments, work with your healthcare provider to develop a safe and gradual plan, whether it’s modifying medication dosages or introducing supplements into your routine.
Your physical and mental health are deeply interconnected. By taking a holistic approach, you can uncover the root causes of your symptoms and unlock better health outcomes. Remember, the key to feeling better may lie in addressing both your thyroid function and mental well-being simultaneously.
Take that first step today—your health is worth it.